Understanding Continence After Robotic Radical Prostatectomy
Why Continence Matters
Robotic radical prostatectomy (RARP) is a highly effective treatment for localised prostate cancer. Although most men regain good bladder control within months, some degree of leakage is common early on. Modern robotic techniques continue to evolve to speed up continence recovery, supported by strong international evidence.
1. Understanding the Anatomy
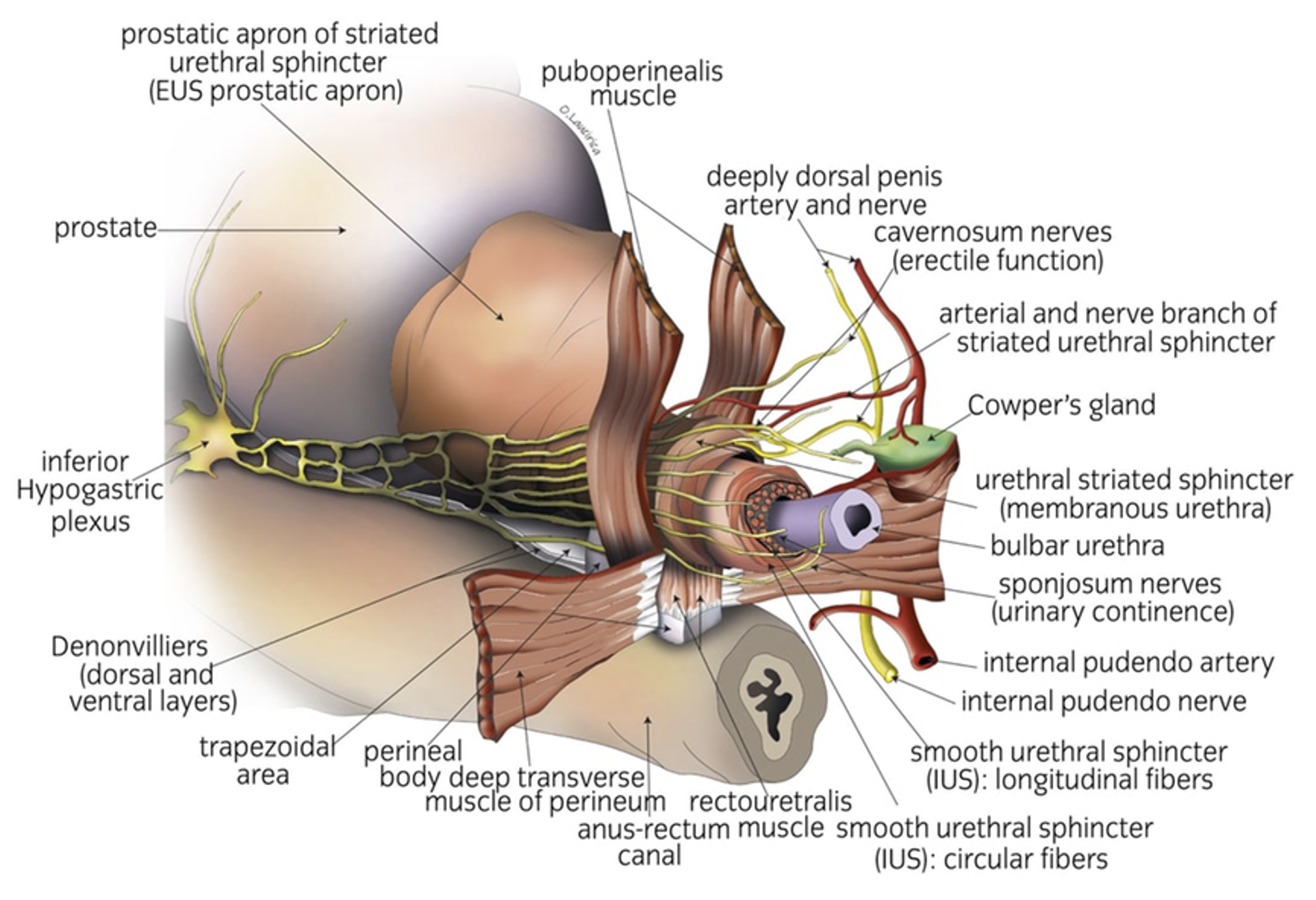
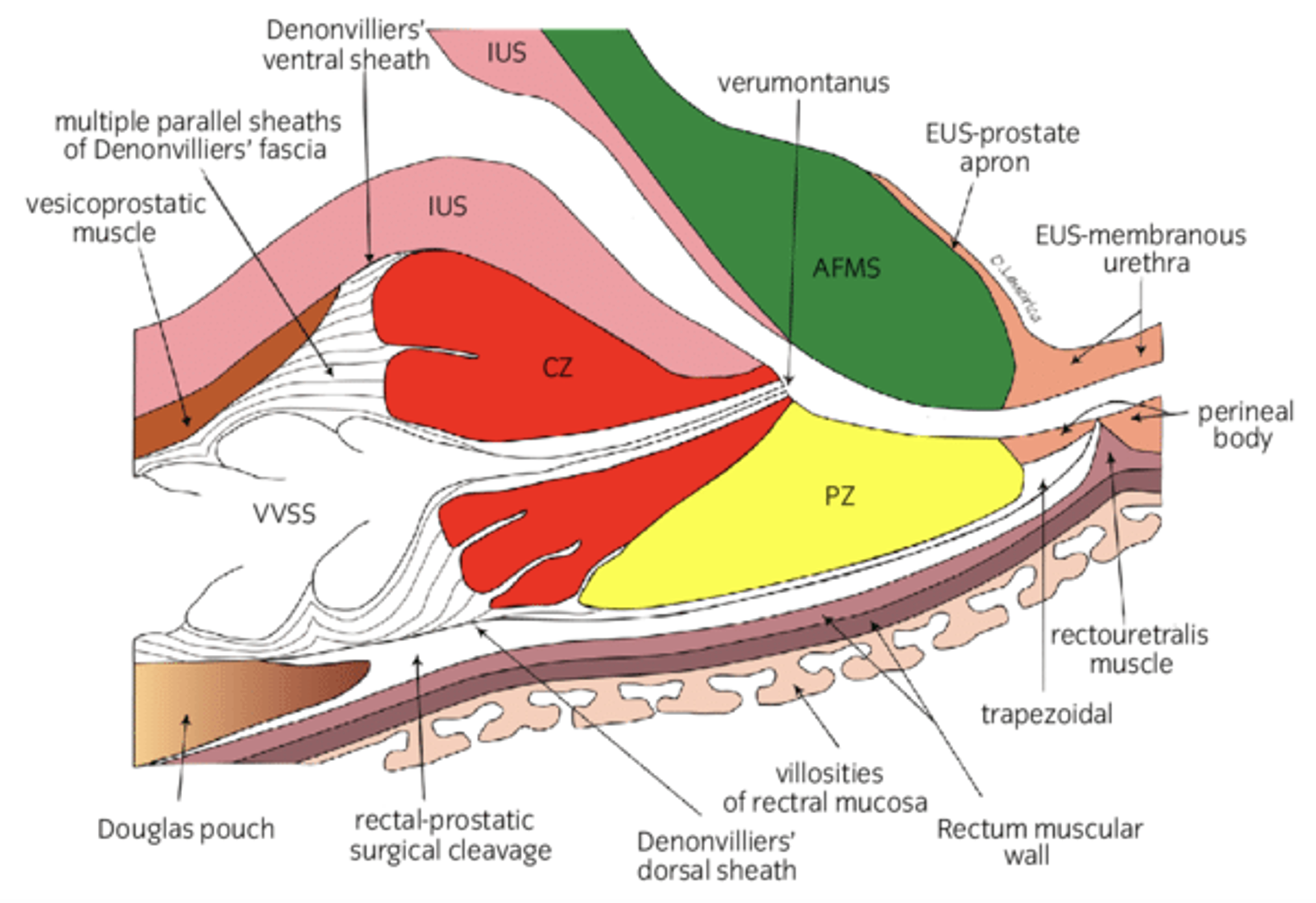
Several key structures help maintain urinary control:
The bladder neck, which acts like a valve
The external urinary sphincter, the main muscle that holds urine
Supportive tissues such as Denonvilliers’ fascia, the puboprostatic ligaments, and the detrusor apron
The neurovascular bundles, important for both erections and fine sphincter function
This image illustrates how preserving the bladder neck, sphincter, supporting tissues and nerves assists continence recovery.
2. How Modern Robotic Surgery Helps Preserve Continence
A. Bladder Neck Preservation (BNP)
Protecting the circular muscle fibres at the bladder base helps:
Faster early continence
Better long-term continence
No increase in cancer-positive margins when performed selectively
Some surgeons also use complete urethral preservation, allowing up to 50% of men to be continent immediately after catheter removal.
B. Nerve-Sparing Techniques
Preserving the neurovascular bundles supports both erectile recovery and early urinary control.
Large studies show:
Better continence within 6 months
Higher continence at 12 months
Modern refinements (e.g., Veil of Aphrodite, PERUSIA technique) demonstrate very high early continence rates.
C. Preserving the External Sphincter and Urethral Length
The more urethral sphincter that is kept intact, the better the continence outcome.
Evidence shows:
Each millimetre preserved improves continence
Careful “subapical” dissection protects the functional sphincter
D. Retzius-Sparing Approach
This technique avoids disturbing the natural supports of the bladder and urethra.
Findings include:
Immediate continence rates >90% in some series
Faster return to bladder control
A slightly higher chance of positive margins in specific tumour locations (e.g., anterior tumours)
E. Reconstructive Techniques
Posterior Reconstruction (Rocco Stitch)
Recreates the supportive “hammock” behind the urethra, improving early continence.
Anterior Reconstruction (Patel Stitch)
Provides suspension and support to the sphincter.
Total Reconstruction
Combines both techniques.
Up to 80% of men are continent at 3 months
Supported by multiple randomised trials
3. Newer Techniques
Single-Port Transvesical Robotic Prostatectomy
A newer approach performed through the bladder using the da Vinci SP system:
96% continence by 3 months
Very short catheter time (about 4 days)
While not widely available yet, it highlights the continued evolution of continence-preserving surgery.
4. What This Means for You
Most men regain good urinary control
Leakage is common in the first few weeks
Most are dry or nearly dry by 3–6 months
Improvement continues up to 12 months and beyond
Your surgeon’s experience matters
The paper repeatedly emphasises that surgeon expertise and training are key to achieving the best continence outcomes.
Why See Dr Osama Al-Bermani
Dr Al-Bermani has been formally trained in the UK in a high-volume ERUS robotic surgery centre, with extensive experience in:
Bladder neck preservation
Advanced nerve-sparing methods
Complete urethral preservation
Retzius-sparing and hood-style techniques
Total anatomical reconstruction for continence support
He will personally walk you through all surgical options, explain which continence-preserving techniques are appropriate for your cancer, and tailor the operation to maximise both cancer control and functional recovery.